
#Skin cancer, #basal cell carcinoma, #Mohs Micrographic Surgery, #screening, #dermatologist
Mohs Micrographic Surgery (MMS) is a highly specialized surgical technique used to treat skin cancers, particularly basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Developed by Dr. Frederic Mohs in the 1930s, MMS has revolutionized the treatment of skin cancer, offering unparalleled accuracy, effectiveness, and cosmetic outcomes.
History of Mohs Micrographic Surgery
Dr. Frederic Mohs, a renowned dermatologist, pioneered MMS in the 1930s. Initially, the technique involved using a zinc chloride paste to fix the tissue, allowing for serial sectioning and examination. Over the years, MMS has evolved, incorporating advancements in microscopy, histopathology, and surgical techniques. Today, MMS is widely regarded as the gold standard for skin cancer treatment.
Principles of Mohs Micrographic Surgery
MMS combines surgical excision with microscopic examination, ensuring complete removal of cancerous tissue while preserving healthy tissue. This involves:
- Surgical excision of the visible tumour
- Processing and sectioning of the tissue
- Microscopic examination of the sections
- Mapping of the tumour margins
- Repeat excision and examination until clear margins are achieved
Indications for MMS include
- High-risk tumours (aggressive subtypes, large size, or location)
- Recurrent tumours
- Tumours in cosmetically sensitive areas (face, hands, feet)
Benefits of Mohs Micrographic Surgery
MMS offers numerous benefits, including:
- High cure rates (up to 99% for primary BCC)
- Minimal tissue removal, preserving cosmetic appearance
- Reduced risk of recurrence
- Improved accuracy, reducing the need for additional surgeries
- Enhanced patient comfort and satisfaction (Performed in an outpatient setting with local anaesthesia. The removal of cancer and repair of the wound is all undertaken in the same day)
Applications of Mohs Micrographic Surgery
MMS is primarily used to treat:
- Basal cell carcinoma (BCC)
- Squamous cell carcinoma (SCC)
- Other rare skin cancers (e.g., Merkel cell carcinoma)
How is Mohs Micrographic Surgery different from conventional cancer removal surgery aka Wide Local Excision?
Mohs Micrographic Surgery (MMS) and Wide Local Excision (WLE) are two surgical techniques used to treat skin cancer. Here are the main differences:
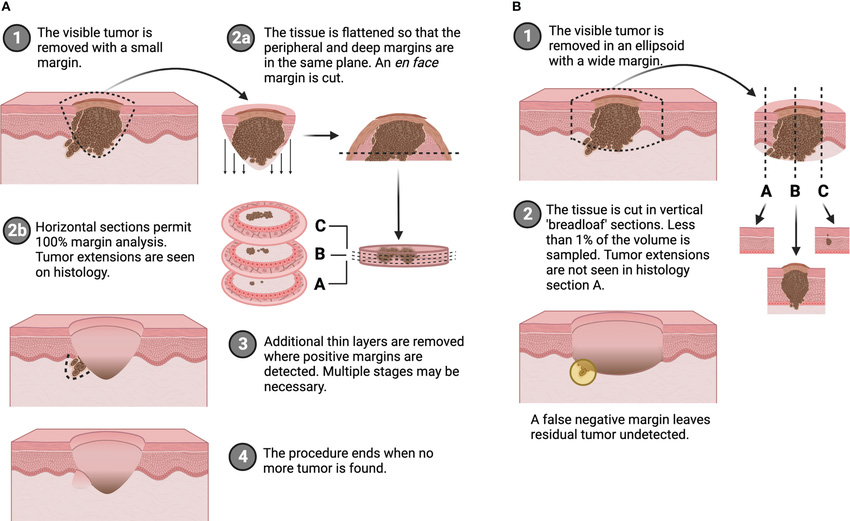
| Mohs Micrographic Surgery | Wide Local Excision | |
| Tissue removal | Removes cancerous tissue in stages, examining each layer under a microscope until clear margins are achieved | Removes a larger area of tissue around the tumour in one go, with a predetermined margin |
| Surgical margin control | Provides 100% margin control, examining the entire tumour margin | Sampling regular sections of tissue to ensure clear margins |
| Tissue Preservation | Narrow margin control allows for healthy tissue preservation, reducing cosmetic impact. | May remove more healthy tissue, potentially leading to larger scars |
| Cure rates | Higher cure rates (up to 99% for primary BCC) | Lower cure rates (around 90% for primary BCC) |
| Surgical Time | Typically longer procedures – performed in stages over several hours | Generally shorter procedures (30 minutes to 1 hour) |
| Specialised training | Requires specialized training and expertise for surgeon and assisting surgical team | Can be performed by a wider range of surgeons |
| Tumour specific factors | Cosmetically sensitive areas (Face, hands, feet) AND/OR high-risk subtype | Low-risk tumours, smaller lesions, or tumours in less critical areas. |
Conclusion
Mohs Micrographic Surgery has transformed the treatment of skin cancer, offering unparalleled accuracy, effectiveness, and cosmetic outcomes. Its evolution over the years has solidified its position as the gold standard for skin cancer treatment in critical skin sites. As skin cancer incidence continues to rise, the importance of MMS in modern dermatological practice cannot be overstated. Patients and healthcare professionals alike can rely on MMS to provide the best possible outcomes for skin cancer treatment.

 Contact us for
Contact us for
 Contact us for
Contact us for